|
Why Exercise is Good Medicine
Author:
Stan Reents, PharmD
Original Posting:
10/19/2012 09:41 AM
Last Revision: 04/19/2020 11:09 AM
In 2017, the RAND Corporation released a report summarizing the prevalence of chronic disease in the US. Based on health statistics from 2014, it reveals: - 60% of adults in the US have at least one chronic disease.
- 42% of adults have more than one chronic disease.
- In adults 65 years and older, 81% have more than one chronic disease.
Most of these health problems are due to a person's lifestyle: smoking, not exercising, poor diet. Thus, "lifestyle"-related illnesses now represent the largest percentage of health care expenses in the US. HEALTH CARE EXPENSES It's not news that the US spends more money on health care per person than any country on earth: The December 1, 2008 issue of TIME magazine contained an evaluation of health care in various countries. At that time, annual health care costs (per capita) in the US were $7026, much higher than other developed countries. Since then, our #1 ranking on that list hasn't changed. An extensive analysis comparing health care in the US to 10 other countries appeared in the March 13, 2018 issue of JAMA (Papanicolas I, et al. 2018):
COUNTRY
(rank) | ANNUAL HEALTH CARE COSTS
PER CAPITA
(2016 data) | | (1) USA | $9403 | | (2) Sweden | $6808 | | (3) Switzerland | $6787 | | (4) Denmark | $6463 | | (5) Netherlands | $5202 | | (11) UK | $3377 |
Yet, we aren't getting the best results (that explains the title of the TIMES article "The Sorry State of American Health"): • In 2005, an analysis of the management of cardiovascular disease in 661 medical centers in 15 countries revealed that the country with the worst blood pressure control, medication compliance, and follow-up rate was.....the US! (Black HR, et al. 2005.) • A 2018 report from the ongoing Global Burden of Disease Study revealed that, whereas mortality rates for adults ages 20-55 had been declining for decades in the US, between 1990 and 2016 mortality rates actually increased in 19 states! In terms of life expectancy, the US ranks a lowly 43rd compared to other countries (Koh HK, et al. 2018). Consider our 2 biggest chronic health problems: cardiovascular disease and obesity. Currently, 121 million adults in the US have some form of cardiovascular disease. That corresponds to 48% of all adults. And 74 million are obese (BMI of 30 and above). If you also include people who are overweight (BMI 25-29), that number increases to 168 million. That's a staggering 71% of all adults! (Virani SS, et al. 2020) Cardiovascular Disease Cigarette smoking has been declining steadily in the US and is now down to 14% (2017 data), its lowest level in decades (Virani SS, et al. 2020). LDL-cholesterol levels and the death rate due to cardiovascular disease (CVD) have also declined steadily during the past 2 decades in the US. But, CVD is still the #1 cause of death of adults. Ominously, in 2010, deaths due to CVD began to increase again (Virani SS, et al. 2020). Why haven't we had better success in managing cardiovascular disease in the US? One answer to that question is that pounding away at cholesterol with cholesterol-lowering drugs isn't as effective for preventing cardiovascular disease as many people believe (de Lorgeril M. 2009): • In the November 8, 2010 issue of the Archives of Internal Medicine, John Pippin, MD, critiqued the JUPITER trial, and summarized a meta-analysis of studies of statin drugs: "These findings suggest that three-fourths of patients who take statins to prevent a first cardiovascular event do not benefit from this treatment." A separate analysis revealed that a disturbingly high 41% of patients had an LDL-cholesterol level of < 100 mg/dL at the time of their first heart attack (myocardial infarction) (Sachdeva A, et al. 2009). This LDL-cholesterol value is generally considered acceptable. In other words, people with "acceptable" cholesterol levels can still have a heart attack. People with diabetes, hypertension, or elevated cholesterol often have more than one of these chronic conditions concurrently. Thus, they need multiple drugs. But, regardless of the effectiveness of drug therapy, patients often don't take their medications as prescribed (this is called "patient compliance"): • Antihypertensive Drugs: An analysis of 4783 patients revealed that almost half had discontinued their blood pressure medication at the end of the first year (Vrijens B, et al. 2008.) • Cholesterol-Lowering Drugs: Numerous studies have documented poor long-term compliance with statins. In one, only 25-40% of patients took their drugs as prescribed during the 2 years they were monitored (Jackevicius CA, et al. 2002.) • Post-MI Drugs: 12% of patients who suffered a myocardial infarction (heart attack) and who were discharged on aspirin, a beta-blocker, and a statin-type cholesterol drug had stopped taking all 3 drugs within the first month! (Ho PM, et al. 2006.) Many patients with coronary artery disease undergo a procedure where a stent (tube) is placed inside the coronary artery to keep it open. Medical terms for this include "intracoronary stent implantation" or "percutaneous coronary intervention" (PCI). Some research shows that performing a PCI procedure isn't very effective: • In 2007, the prestigious New England Journal of Medicine published a report stating "...PCI did not reduce the risk of death, myocardial infarction, or other major cardiovascular events when added to optimal medical therapy." (Boden WE, et al. 2007). • The January 23, 2012 issue of the Archives of Internal Medicine included a study showing that nearly 1 in 10 cardiac patients who undergo a PCI required readmission to the hospital within 30 days (Khawaja FJ, et al. 2012). Obviously, those aren't glowing endorsements of this procedure! Obesity In terms of number of people affected, obesity (defined as a BMI of 30 or higher) is now the #1 chronic health problem in the US. The latest statistics show the following (Flegal KM, et al. 2016) (Ogden CL, et al. 2016) (Virani SS, et al. 2020):
| GROUP | PERCENT OBESE | | Men | 36% obese | | Women | 40% obese | | Adolescents | 20% obese |
These are the worst obesity rates we've ever seen in the US. A 2012 report from the Robert Wood Johnson Foundation ("F as in Fat: How Obesity Threatens America's Future 2012") projects that by 2030, obesity rates will exceed 44% in all 50 states and will add another $48-66 billion to the cost of treating obesity-related disease (Voelker R. 2012). Consequences of Obesity: • Type-2 diabetes is a close companion of obesity. Obesity is getting worse, but type-2 diabetes is increasing even more rapidly: Between 1990 and 2016, diabetes increased in almost every state in the US (Koh HK, et al. 2018). • Low-grade inflammation exists in people who are obese. Many years of low-grade inflammation contributes to a wide variety of chronic diseases. Cardiovascular disease and obesity affect tens of millions of Americans. Health care expenses for both are projected to continue to rise during the next several decades. If we could reduce the development of atherosclerosis (the cause of cardiovascular disease) and obesity, we would see a huge decrease in the amount of chronic disease in the US. We need to consider a different approach to chronic health problems like these... THE POWER OF PREVENTION One glaring deficit in the health care system in the US is how little time, money, and effort is placed on preventive care. The TIME magazine review from 2008 gave "Preventive Care" in the US a grade of D+. The March 13, 2018 analysis from JAMA revealed that only 3% of our health care expenses are devoted to Preventive Care (Papanicolas I, et al. 2018). Instead, we pursue a strategy based on drug therapy and expensive procedures which only address the symptoms of the problem. Professor Steven Blair has recently concluded that "physical inactivity is the biggest public health problem of the 21st century." After analyzing nearly 54,000 patients, he shows that: "Low cardiorespiratory fitness" was the biggest contributor to death than any of the other traditional risk factors that clinical medicine currently monitors. 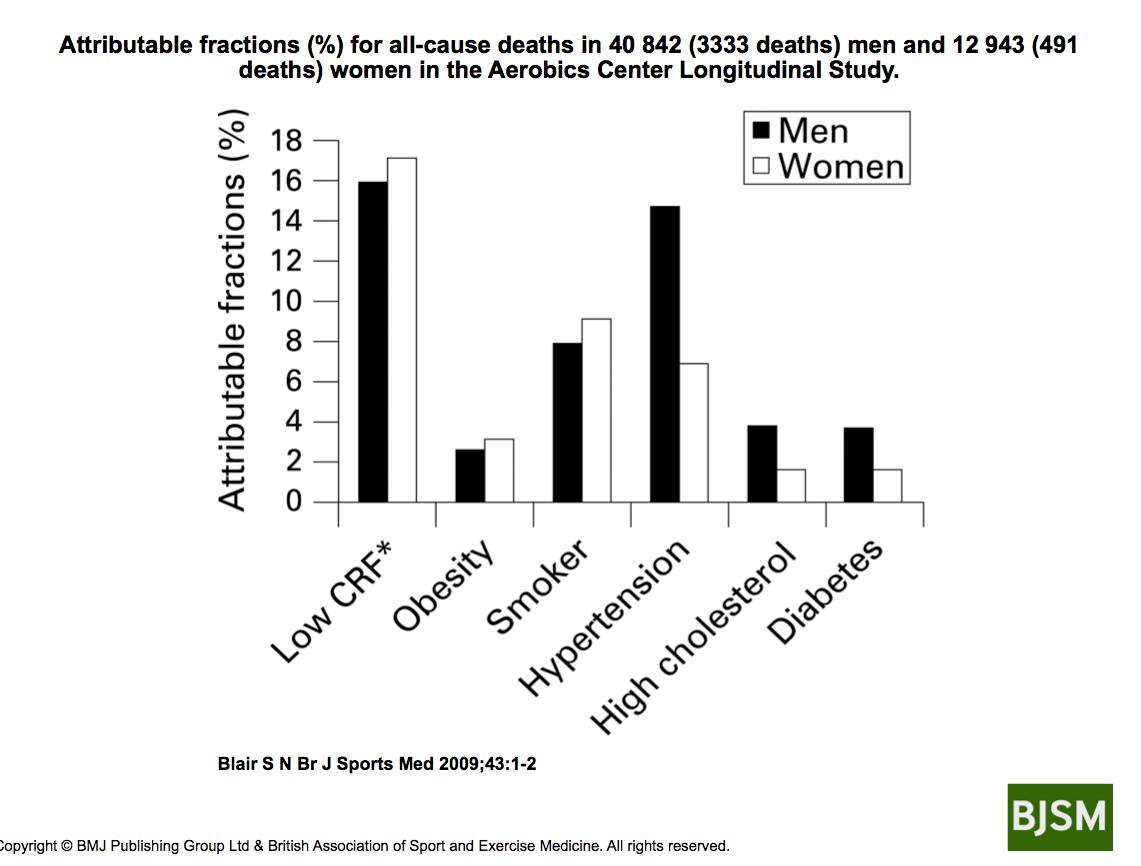
In fact, "low cardiorespiratory fitness" was a substantially higher determinant of death than risk factors that currently get most of the attention such as obesity and elevated cholesterol (Blair SN. 2009.) What he is saying here is that your fitness level is more important than your cholesterol level! 
EXERCISE REALLY IS A THERAPEUTIC AGENT! The title of an editorial by William Roberts, MD, in the American Journal of Cardiology illustrates how versatile exercise is: “An agent with lipid-lowering, antihypertensive, positive inotropic, negative chronotropic, vasodilating, diuretic, anorexigenic, weight-reducing, cathartic, hypoglycemic, tranquilizing, hypnotic and antidepressive qualities.” That's pretty impressive, isn't it? The "agent" he is describing here is aerobic exercise. What's also impressive is that this paper was published in 1984.... that was more than 30 years ago! Today, the title could also include: "memory-enhancing," "cancer-preventing," "anti-arthritic," and "clot-preventing" as well! Is exercise really that effective for prevent serious medical conditions? Yes. A great deal of research now documents the effectiveness of exercise in a wide variety of human diseases. Bente Pedersen, MD, and Bengt Saltin, MD, published a review of 26 diseases that exercise can be used in. This paper is 72 pages long and cites nearly 800 research studies! (Pedersen BK, et al. 2015). Our Articles Library provides detailed reviews on many of these conditions, but, briefly: Exercise Prevents Cardiovascular Disease: Regular exercise substantially lowers the risk of developing cardiovascular diseases such as coronary artery disease, hypertension, stroke, heart failure, intermittent claudication. • Running Prevents Atherosclerosis: Paul T. Williams, PhD, at the Lawrence Berkeley National Laboratory in Berkeley, CA, analyzed health data on more than 107,000 runners in The National Runners' Health Study. Distance runners (Williams PT, et al. 2007) and marathon runners (Williams PT. 2009) required drug therapy for cholesterol, diabetes, and/or hypertension less frequently compared to those who didn't run this much. • Walking Prevents Atherosclerosis: Then, he discovered that walking reduced the risk of developing diabetes, hypertension, and elevated cholesterol similar to the benefits of running (Williams PT, et al. 2013), and that walkers were also less likely to require prescription drugs for these conditions (Williams PT. 2008). On the other hand, young adults with poor aerobic fitness are 3 to 6 times more likely to develop diabetes, hypertension, and the metabolic syndrome compared to people with very good aerobic fitness (Carnethon MR, et al. 2003). The same pattern has been documented in older men (Sesso HD, et al. 2000) and older women (Kokkinos PF, et al. 1995). Exercise Helps to Prevent Obesity: Regular exercise helps to prevent obesity. But, here, diet is the most important factor. Exercise Prevents Metabolic Disease: Regular exercise is nearly a mandatory strategy for preventing type-2 diabetes, elevated lipids, and metabolic syndrome. Exercise Prevents Musculoskeletal Disease: Teenage girls who perform the right types of exercise, and in the right amount, develop better bone density. This advantage exists for the rest of their lives, thus reducing the risk of complications of osteoporosis. Regular exercise and less sitting reduce simple back pain, a problem that affects 80% of adults at some point in their life. Exercise Prevents Mental Health Problems: People who exercise regularly have lower rates of anxiety and depression. Regular exercise improves mental performance at work and in the classroom. And regular exercise can lower the risk of developing some forms of dementia. Exercise Reduces the Risk of Various Forms of Cancer: Regular exercise can reduce the risk of several types of cancer. Exercise -- along with a plant-based diet -- is critical for preventing chronic medical problems! IN SOME CASES, EXERCISE IS BETTER THAN DRUG THERAPY In 2013, Huseyin Naci and John Ioannidis, MD, at Stanford analyzed 305 randomized controlled clinical trials involving over 339,000 patients. They compared the response to exercise versus the response to drug therapy (Naci H, et al. 2013):
| MEDICAL CONDITION | EXERCISE vs. DRUG THERAPY | Coronary Artery Disease
(secondary prevention of) | Exercise is as good as Drug Therapy | Diabetes
(prevention of) | Exercise is as good as Drug Therapy | Stroke
(rehab of) | Exercise is BETTER THAN Drug Therapy | Congestive Heart Failure
(treatment of) | Drug Therapy is better than Exercise |
Exercise and the "Risk Factor Gap" in Cardiovascular Disease Atherosclerosis is not simply a problem of too much cholesterol (de Lorgeril M. 2009). Rather, atherosclerosis is the result of a variety of physiologic and biochemical disruptions working together to damage the inside surface of the walls of arteries. In addition to the accumulation of cholesterol, other problems co-exist in most people: elevated glucose, elevated blood pressure, elevated triglycerides, and a prolonged state of low-grade inflammation. This is why cholesterol-lowering drugs are not as effective as aerobic exercise: statin-type cholesterol drugs only address 2 of those problems: elevated cholesterol, and they appear to reduce the intensity of low-grade inflammation. But, they do nothing for elevated glucose, they don't lower blood pressure, they don't promote weight loss... ...And they don't provide the myriad of other health benefits that aerobic exercise does. It turns out that exercise (particularly when aerobic fitness is maintained!) is more beneficial for lowering the risk of cardiovascular disease than is predicted by the improvements in traditional risk factors (eg., cholesterol, blood pressure, glucose, triglycerides). This phenomenon is called the "Risk Factor Gap". • Harvard's Women's Health Study revealed that improvements in "traditional" cardiovascular disease risk factors accounted for only 59% of the benefit of regular exercise. This means that exercise provides an additional 41% of health benefits that aren't being measured by your physician. And when they looked at coronary artery disease (a sub-type of the more general category of cardiovascular disease), the "additional" benefits of exercise were even more profound (Mora S, et al. 2007). In fact, it's been shown that an 8-week exercise program improved the health of the vascular system even though cholesterol levels didn't change (Green DJ, et al. 2003). Bottom line? Aerobic exercise improves dozens of physiologic and biochemical variables, easily trouncing the 2 benefits of statin-type cholesterol-lowering drugs. IN SOME CASES, EXERCISE IS BETTER THAN MEDICAL PROCEDURES A striking example where exercise is a more effective therapeutic option than a medical procedure is the setting of coronary artery disease: Researchers in Germany have shown that it is more effective to put patients who have had a heart attack on an exercise program than to perform a PCI procedure: • Patients were given 1 of 2 different treatments after routine coronary angiography: One group rode a stationary bicycle for 20-min per day, combined with one 60-min group exercise session per week. The other group underwent a PCI. After 12 months, the group that exercised had a higher "event-free survival" rate than the group that received the PCI. Further, health care costs in the group that exercised were half the costs in the group that received PCI (Hambrecht R, et al. 2004). Yes, exercise IS good medicine!  MEDICAL GROUPS ENDORSE EXERCISE Because of this, virtually all major medical advisory groups now endorse exercise as a viable health-promoting strategy: • November 2007: The American College of Sports Medicine (ACSM) and the American Medical Association (AMA) jointly launched the “Exercise Is Medicine” initiative. This campaign calls on all physicians to “prescribe” exercise as they would for other traditional therapeutic agents. • June 2008: The US Government's Dept. of Health and Human Services issued its first set of Physical Activity Guidelines. • May 2010: The National Physical Activity Plan was released. Healthy People has been providing exercise / physical activity recommendations for decades. "STEPS" YOU SHOULD TAKE So, what can you do with all this information? Exercise or do some form of physical activity every day! But, first, a couple precautionary statements: 1) If you have any pre-existing medical condition, check with your personal physician before beginning any new exercise routine. 2) If you are currently taking medications, do NOT stop taking them without conferring with your physician. 3) Then, consider starting by going for a walk....if not every day, then, 3-5 days per week. But, eventually try to do it every day. Walk briskly and swing your arms. Try to push your heart rate up a bit. Learn how to monitor your heart rate while you are exercising. Slow down if you get out of breath, and, certainly, stop immediately if you develop chest pain! 4) Periodically, assess your progress by determining your resting heart rate first thing when you wake up. That's it! Yes, it really is that simple to improve your health. You may find that your blood pressure and your cholesterol start to improve, and, you just might lose a little weight. SUMMARY Health care expenses (per capita) in the US are the highest in the world. Yet, we don't have the best health, or, health care. Chronic diseases are the biggest category of health care expenses. Much of this disease is preventable, yet we only direct 3% of our health care dollars to Preventive Care. Exercise is one strategy that could make a huge impact on the health of Americans, and, in turn, health care costs, particularly for chronic diseases such as obesity, diabetes, hypertension, coronary artery disease, etc. What would happen if we focused more attention on exercise as a therapeutic agent in health care? Answer: We might have a better impact on cardiovascular diseases, obesity, type-2 diabetes, the general health of our entire population, and, a reduction in health care expenses!  FOR MORE INFORMATION An entire chapter in Reents' text Sport and Exercise Pharmacology is devoted to the concept of prescribing exercise to "treat" health problems. (This book was published 7 years before the ACSM/AMA "Exercise Is Medicine" initiative was launched!) Readers may also be interested in these reviews: EXPERT HEALTH and FITNESS COACHING Stan Reents, PharmD, is available to speak on this and many other exercise-related topics. (Here is a downloadable recording of one of his Health Talks.) Contact him through the Contact Us page. REFERENCES Black HR, Elliott WJ, Grandits G, et al. Results of the Controlled ONset Verapamil INvestigation of Cardiovascular Endpoints (CONVINCE) trial by geographical region. J Hypertens 2005;23:1099-1106. Abstract Blair SN. Physical inactivity: The biggest public health problem of the 21st century. Br J Sports Med 2009;43:1. Abstract Boden WE, O'Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007;356:1503-1516. Abstract Carnethon MR, Gidding SS, Nehgme R, et al. Cardiorespiratory fitness in young adulthood and the development of cardiovascular disease risk factors. JAMA 2003;290:3092-3100. Abstract de Lorgeril M. Disappointing recent cholesterol-lowering drug trials: Is it not time for a full reappraisal of the cholesterol theory? World Rev Nutr Diet 2009;100:80-89. (no abstract ) Flegal KM, Kruszon-Moran D, Carroll MD, et al. Trends in obesity among adults in the United States, 2005 to 2014. JAMA 2016;315:2284-2291. Abstract Green DJ. Exercise training as vascular medicine: Direct impacts on the vasculature in humans. Exercise Sports Science Reviews 2009;37:196-202. Abstract Green DJ, Walsh JH, Maiorana A, et al. Exercise-induced improvement in endothelial dysfunction is not mediated by changes in CV risk factors: Pooled analysis of diverse patient populations. Am J Physiol Heart Circ Physiol 2003;285:H2679-H2687. Abstract Hambrecht R, Walther C, Mobius-Winkler S, et al. Percutaneous coronary angioplasty compared with exercise training in patients with stable coronary artery disease. Circulation 2004;109:1371-1378. Abstract Ho PM, Spertus JA, Masoudi FA, et al. Impact of medication therapy discontinuation on mortality after myocardial infarction. Arch Intern Med 2006;166:1842-1847. Abstract Ioannidis JPA. More than a billion people taking statins? Potential implications of the new cardiovascular guidelines. JAMA 2014;311:463-464. Abstract Jackevicius CA, Mamdani M, Tu JV. Adherence with statin therapy in elderly patients with and without acute coronary syndromes. JAMA 2002;288:462-467. Abstract Khawaja FJ, Shah ND, Lennon RJ, et al. Factors associated with 30-day readmission rates after percutaneous coronary intervention. Arch Intern Med 2012;172:112-117. Abstract Koh HK, Parekh K. Toward a United States of Health: Implications of understanding the US Burden of Disease. JAMA 2018;319:1438-1440. (no abstract) Kokkinos PF, Holland JC, Pittaras AE, et al. Cardiorespiratory fitness and coronary heart disease risk factor association in women. J Am Coll Cardiol 1995;26:358-364. Abstract Mora S, Cook N, Buring JE, et al. Physical activity and reduced risk of cardiovascular events. Potential mediating mechanisms. Circulation 2007;116:2110-2116. Abstract Naci H, Ioannidis JPA. Comparative effectiveness of exercise and drug interventions on mortality outcomes: Metaepidemiological study. Br Med J 2013;347:f5577. Abstract Ogden CL, Carroll MD, Lawman HG, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. JAMA 2016;315:2292-2299. Abstract Papanicolas I, Woskie LR, Jha AK. Health care spending in the United States and other high-income countries. JAMA 2018;319:1024-1039. Abstract Pedersen BK, Saltin B. Evidence for prescribing exercise as therapy in chronic disease. Scan J Med Sci Sports 2006;16(suppl. 1):3-63. Abstract Pedersen BK, Saltin B. Exercise as medicine. Evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports 2015;25(Suppl. 3):1-72. Abstract Roberts WC. An agent with lipid-lowering, antihypertensive, positive inotropic, negative chronotropic, vasodilating, diuretic, anorexigenic, weight-reducing, cathartic, hypoglycemic, tranquilizing, hypnotic and antidepressive qualities. Am J Cardiol 1984;53:261-262. Abstract Sachdeva A, Cannon CP, Deedwania PC, et al. Lipid levels in patients hospitalized with coronary artery disease: An analysis of 136,905 hospitalizations in Get With The Guidelines. Am Heart J 2009;157:111-117. Abstract Sesso HD, Paffenbarger RS, Lee I-M. Physical activity and coronary heart disease in men. The Harvard Alumni Health Study. Circulation 2000;102:975-980. Abstract Virani SS, Alonso A, Benjamin EJ, et al. Heart disease and stroke statistics 2020 update: A report from the American Heart Association. Circulation 2020;141:e139-e596. Abstract Voelker R. Escalating obesity rates pose health, budget threats. JAMA 2012;308:1514. (no abstract) Vrijens B, Vincze G, Kristanto P, et al. Adherence to prescribed antihypertensive drug treatments: Longitudinal study of electronically compiled dosing histories. Br Med J 2008;336:1114-1117. Abstract Williams PT. Reduced diabetic, hypertensive, and cholesterol medication use with walking. Med Sci Sports Exerc 2008;40:433-443. Abstract Williams PT. Lower prevalence of hypertension, hypercholesterolemia, and diabetes in marathoners. Med Sci Sports Exerc 2009;41:523-529. Abstract Williams PT, Franklin B. Vigorous exercise and diabetic, hypertensive, and hypercholesterolemia medication use. Med Sci Sports Exerc 2007;39:1933-1941. Abstract Williams PT, Thompson PD. Walking versus running for hypertension, cholesterol, and diabetes mellitus risk reduction. Arterioscler Thromb Vasc Biol 2013;33:1085-1092. Abstract ABOUT THE AUTHOR 
Stan Reents, PharmD, is a former healthcare professional. He is a member of the American College of Lifestyle Medicine (ACLM) and a member of the American College of Sports Medicine (ACSM). In the past, he has been certified as a Health Fitness Specialist by ACSM, as a Certified Health Coach by ACE, as a Personal Trainer by ACE, and as a tennis coach by USTA. He is the author of Sport and Exercise Pharmacology (published by Human Kinetics) and has written for Runner's World magazine, Senior Softball USA, Training and Conditioning and other fitness publications.
Browse By Topic:
aerobic exercise, coronary artery disease, depression, diabetes, drug therapy, exercise and health, exercise recommendations, health care costs, heart disease, hypertension, obesity, osteoporosis, walking
Copyright ©2026 AthleteInMe,
LLC. All rights reserved.
|